The pandemic has driven advances in all aspects of disease prevention from the basics of hand hygiene and surface cleaning and disinfection, to social distancing and acceleration of vaccine development and production.
However, there are still many other bacteria, virus’ and fungi that need to be eliminated to best protect patients, healthcare staff and the wider population. If we focus just on COVID-19 and things such as disinfectant contact times and efficacy only for COVID-19, we risk not suitably managing these other pathogens, which will lead to increased adverse health outcomes and morbidity.
Candida auris (C.auris) is a fungus from the same group of germs that cause thrush (Candida albicans) or serious blood stream infections in immune-compromised patients (C. glabrata, C. parapsilosis, C. krusei and C. tropicalis).
Unlike most of the other candida species which live in the gastrointestinal tract, this fungus is also commonly found living on the skin. It is much more resistant than other fungi to commonly used treatments and over 90 per cent of C.auris cases to date have been resistant to Fluconazole, the standard treatment for Candida infections.
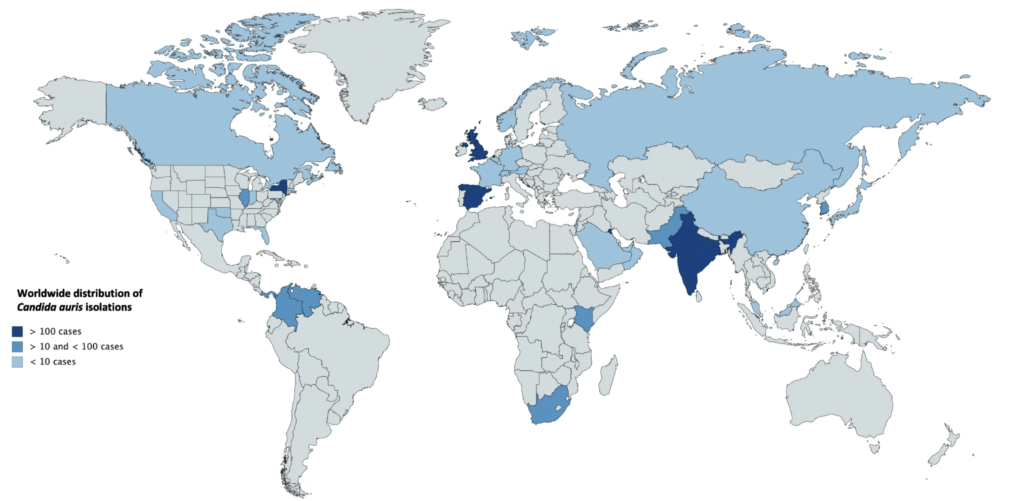
Multi-resistant C.auris has only emerged relatively recently; it was first identified in Japan and South Korea in 2009 but had spread to six continents by 2017. C.auris is of particular interest to clinicians, infectious disease experts and infection prevention and control (IPC) professionals due to the following characteristics of the fungus:
- It’s a pathogen – it causes disease
- It’s of risk to all types of patients
- It’s often mis-classified in laboratory diagnostic tests
- There are few treatment options
- It spreads easily in the environment
- It’s resilient to environmental disinfection
Healthcare facility outbreaks
As with many other antimicrobial resistant pathogens, C. auris has been implicated in many hospital outbreaks around the world. A large outbreak lasting over 12 months between 2015 and 2016 in a London cardiothoracic intensive care unit resulted in 50 cases. Contact with an environment contaminated with C. auris was found to be a significant source of infection with the fungus.
Infection prevention and control measures
C.auris cases should be taken very seriously in all healthcare facilities and strict measures put in place to prevent spread to other patients.
These measures are similar to other important IPC practices for multi-drug resistant organisms and include the following key actions:
- Notify local IPC and infectious diseases experts
- Place patient in single room with contact and isolation precautions
- For symptomatic disease, begin treatment, with guidance from an infectious disease specialist (treatment of asymptomatic colonisation is not recommended)
- Contact tracing and screening to determine local transmission
- Focus on environmental disinfection
Disinfection of a contaminated environment
Removing C.auris from environments is a challenge due to the ease which it spreads and its resistance to common cleaning agents. The environment can remain contaminated for weeks. Subsequently many guidelines for the management of these infections, advise daily and terminal or discharge cleaning with a strong environmental disinfectant such as a sporicidal disinfectant.
As with all environmental disinfection options, success will be easier if the area is regularly cleaned so that surface biofilm is not allowed to build up. Importantly as with other pathogens ensuring suitable contact time exposure to the disinfectant and sporicidal agent is essential in effective outcomes and pathogen reduction.
Summary
Multi-drug resistant Candida auris is an important pathogen which demands attention and action when identified in the healthcare setting. As well as implementing common IPC measures, disinfection of a potentially contaminated environment must be a priority.
Always follow requisite guidelines for managing this pathogen and ensure contact times are enforced, noting that for any disinfectant or sporocidal agent the contact times against different pathogens may vary.
References:
Schelenz, Silke, et al. “First hospital outbreak of the globally emerging Candida auris in a European hospital.” Antimicrobial Resistance & Infection Control 5.1 (2016): 35.
Schwartz, Smith & TC Dingle. “Something wicked this way comes: What health care providers need to know about Candida auris”. Can Commun Dis Rep (2018);44(11):271–6.